Assessment of Infection and Colds (PCS3)
The table below lists the virological measures and assessments of objective cold signs and subjective cold symptoms that were collected in PCS3. Data derived from these measures were used to determine infection with the challenge virus and subsequent development of clinical upper respiratory illness. The criteria used for identifying infection and illness are described in detail below.
| Category | Specific Measure |
| Virology | |
| serum | Baseline & Post-Challenge Virus-Specific Ab in Serum |
| nasal secretions | Isolation and Confirmation of Challenge Virus |
| nasal secretions | Quantification of Challenge Virus |
| Objective Cold Signs | |
| nasal congestion | Nasal Mucociliary Clearance Function |
| mucus production |
Nasal Mucus Weights |
| Subjective Cold Symptoms | Self-Report (questionnaire) |
Infection
A necessary precondition for identifying participants who developed clinical upper respiratory illness was verified infection with the challenge virus. To determine whether participants had become infected subsequent to challenge, all 5 studies employed criteria described by Gwaltney and colleagues (1989) that involved evidence of viral replication (shedding) and/or changes in serum specific antibody titer. Specifically, participants were considered to be infected with the challenge virus if either of the following two conditions had been met:- Recovery of the challenge virus in nasal secretions on any of the post-challenge days
- A 4-fold or greater increase in the virus-specific antibody titer between the pre-viral challenge baseline (3 to 5 days before viral challenge) and 28 days post-challenge1
Upper Respiratory Tract Involvement
PCS3 used two sets of criteria to determine the presence of upper respiratory tract involvement, with the first being based on participants’ self-reports of perceived physical symptoms and the second on objectively assessed signs of upper respiratory pathology. Henceforth, we will refer to these as the subjective definition (or subjective criteria) and the objective definition (or objective criteria), respectively. The subjective criteria have been used widely in the virology literature. We prefer the objective criteria because they focus on observable disease pathology and thus completely eliminate any possibility that the outcome reflects biases in how individuals perceive or report their bodily sensations. Again, we emphasize that satisfaction of the sign and symptom criteria discussed below is suggestive of clinical illness only in the context of a verified infection.Criteria for Objective Signs of Upper Respiratory Pathology
Using the objective criteria (Cohen et al., 1997), participants were determined to have developed a clinical cold if they were both infected with the challenge virus and met either of the following criteria:- Total baseline-adjusted mucus weight (i.e., summed across all post-challenge days) of 10g or more
- Average (across all post-challenge days) baseline-adjusted nasal mucociliary clearance time of 7 minutes or longer (or total clearance time across 5 post-challenge days of 35 minutes or longer, as reported in some publications).
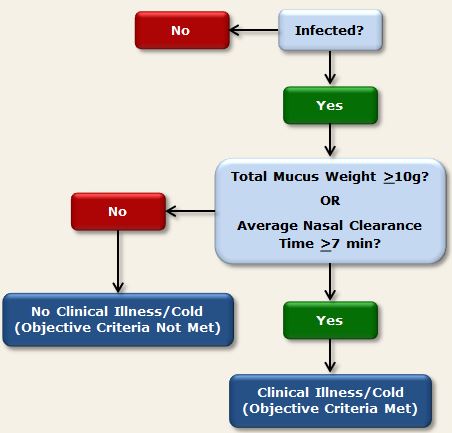
Figure 1. Objective criteria used in PCS3 to determine clinical illness
Criteria for Subjective Upper Respiratory Symptoms
We have favored the objective criteria for upper respiratory involvement described above because subjective assessments of symptoms and illness may be influenced by psychological variables. Such effects may occur independent of any influence of the objective signs of disease. However, historically, virologists studying risk factors for colds have used subjective criteria. Here we describe the modified Jackson Criteria (Gwaltney, Moskalski, & Hendley, 1980), which take into account individuals’ subjective ratings of 8 respiratory symptoms identified by Jackson and colleagues (1958) as being characteristic of the common cold. Importantly, satisfaction of subjective upper respiratory symptom criteria is suggestive of clinical illness only in the context of a verified infection.Daily symptom reports
At the end of each day in quarantine, participants used a scale ranging from 0 (none) to 4 (very severe) to rate their experience during the past 24 hours of each of the following 8 symptoms of upper respiratory illness (see Daily Symptoms):- nasal congestion
- runny nose
- sneezing
- cough
- sore throat
- malaise (feeling “under the weather”)
- headache
- chills
In addition to rating the severity of these 8 symptoms, participants were asked each day whether they thought that had a cold or flu.
Jackson Symptom Scores
Symptom severity ratings were summed within each day to create a daily Jackson Symptom Score (possible range, 0 to 32). Adjusted Daily Jackson Symptom Scores were computed by subtracting the DAY 0 (pre-challenge) Jackson Symptom Score from the Jackson Score reported on each subsequent post-challenge day. Adjusted scores were then averaged across all post-challenge days to create a Total Adjusted Jackson Symptom Score.Modified Jackson Criteria
In the 4 cold studies that collected subjective symptom data, the Modified Jackson Criteria were used to determine whether participants’ subjective assessments of their cold symptoms were consistent with a diagnosis of clinical upper respiratory illness. These criteria are defined as- having a Total Adjusted Jackson Symptom Score of 6 or more AND
- reporting having a cold or flu on any post-challenge quarantine day OR reporting rhinorrhea on 3 or more post-challenge days.2
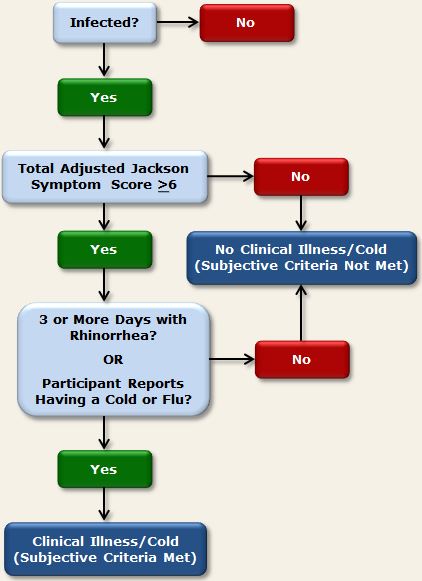
Figure 2. Subjective criteria used in PCS3 to determine clinical illness
Notes
1 In addition to the baseline and post-challenge samples, PCS3 included a screening sample that was collected 2 months prior to viral challenge. Based on this sample, volunteers were excluded from participation if their serum specific Ab titers were >4.
2 Symptom ratings used in the creation of the original Jackson criteria (Jackson et al., 1958) were rated on a scale of 0 to 3, and the criterion score was a total of 14 points over a post-challenge observation period of 6 days. As with the modified criteria, individuals also had to report having a cold or experiencing 3 or more days with rhinorrhea.
References
Cohen, S., Doyle, W. J., Turner, R. B., Alper, C. M., & Skoner, D. P. (2003). Emotional style and susceptibility to the common cold. Psychosomatic Medicine, 65, 652-657.Cohen, S., Doyle, W. J., Skoner, D. P., Rabin, B. S., & Gwaltney, J. M., Jr. (1997). Social ties and susceptibility to the common cold. Journal of the American Medical Association, 277, 1940-1944.
Gwaltney, J. M. Jr., Colonno, R. J., Hamparian, V. V., & Turner, R. B. (1989). Rhinovirus. In N. J. Schmidt & R. W. Emmons (Eds). Diagnostic procedures for viral, rickettsial, and chlamydial infections, 6th ed (pp. 579-614). Washington, D.C.: American Public Health Association.
Gwaltney, J. M. Jr., Moskalski, P. B., & Hendley, J. O. (1980). Interruption of experimental rhinovirus transmission. Journal of Infectious Diseases, 142, 811-815.
Jackson, G. G., Dowling, H. F., Spiesman, I. G., & Boand, A. V. (1958). Transmission of the common cold to volunteers under controlled conditions. I. The common cold as a clinical entity. Archives of Internal Medicine, 101, 267-278.