New Gene-Editing Technology Cures a Genetic Blood Disorder in Mice
The technology may offer a minimally invasive treatment for genetic disorders of the blood
By Jocelyn Duffy
PITTSBURGH – A next-generation gene-editing system developed by Carnegie Mellon University and Yale University scientists has successfully cured a genetic blood disorder in living mice using a simple IV treatment. Unlike the popular CRISPR gene-editing technique, the new technology can be administered to living animals and it significantly decreases unwanted, off-target gene mutations. The findings, reported in Nature Communications, offer a new therapeutic approach to treat genetic diseases of the blood like beta thalassemia and sickle cell disease by targeting faulty genes in hematopoietic stem cells.
The novel system relies on state-of-the-art peptide nucleic acid (PNA) molecules, a synthetic nucleotide technology that has been pioneered at Carnegie Mellon’s Center for Nucleic Acids Science and Technology (CNAST).
“We have developed a system that uses FDA-approved nanoparticles to deliver our PNA molecule along with a donor DNA to repair a malfunctioning gene in living mice. This has not been achieved with CRISPR,” said Danith Ly, professor of chemistry in Carnegie Mellon’s Mellon College of Science and an expert in PNA chemistry.
Gene-editing technologies like CRISPR rely on DNA-cutting enzymes to slice open DNA at a target site to edit a specific gene. The problem with this is twofold. First, the enzymes are large and therefore difficult to administer directly to living animals, so scientists typically remove the cells, treat them in the lab and then put them back into the body. Second, once inside a cell, the enzymes could indiscriminately cut DNA at sites other than the original gene target.
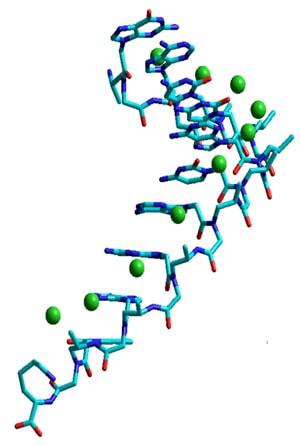
The new Carnegie Mellon/Yale system avoids both of these issues. The new system consists of biocompatible nanoparticles containing PNAs, small nano-sized synthetic molecules in which a protein-like backbone is combined with the nucleobases found in DNA and RNA. PNA is designed to open up double-stranded DNA and bind near the target site in a highly specific manner without cutting anything. And the PNAs easily fit inside the nanoparticle delivery system, which is FDA-approved and has already been used to treat neurodegenerative diseases in humans.
In the latest research, Ly and a former graduate student Raman Bahal designed a PNA to target the malfunctioning gene in beta thalassemia, a blood disorder that reduces the production of hemoglobin. Less hemoglobin leads to a lack of oxygen throughout the body, which can cause a host of problems including pale skin, weakness, fatigue, and more serious complications.
Together with Peter Glazer’s team at Yale, the researchers loaded up the nanoparticles with the PNAs, a donor strand of DNA encoding the sequence for a functional hemoglobin subunit beta (HBB) gene and a stem cell factor that enhances gene editing. When the PNA binds to the target site in the DNA, it forms a PNA-DNA-PNA triplex, leaving a displaced DNA strand. Formation of such a complex enables the donor DNA to bind to the faulty DNA site within the vicinity. Taken together, this altered helix engages the cell’s own DNA repair pathways to correct the malfunctioning HBB gene.
In addition to testing the system on both mouse and human bone marrow stem cells in the lab, the research team also administered the fully-loaded nanoparticles intravenously to mice models of beta thalassemia. The results showed up to 7 percent successful gene editing in hematopoietic stem cells and an elevated level of hemoglobin for several months after treatment. This represented a striking increase over typical gene editing methods that produce only a 0.1 percent success rate.
“The effect may only be 7 percent, but that’s curative,” Ly said. “In the case of this particular disease model, you don’t need a lot of correction. You don’t need 100 percent to see the phenotype return to normal.”
According to the researchers, this work yields two key advances for gene editing. The first is the PNA itself. Ly used next-generation PNA chemistry to design a PNA molecule called a gamma-PNA with a polyethylene glycol group on the side chain. This innovation makes the PNA water-soluble and biocompatible, which means that it doesn’t bind to proteins and other biomolecules in a non-specific manner. Additionally, the specific stereochemistry of the polyethylene glycol group pre-organizes the PNA into a right-handed helical motif, making it bind to DNA more readily. The second advance is the finding that the addition of the stem cell factor promotes increased gene editing.
Ly acknowledged that such work would not be possible without the support of and contribution from his colleagues in CNAST and the generous financial support from the DSF Charitable Foundation that “enabled him the freedom to innovate and pursue far-reaching scientific problems, such as the development of molecular therapy that would one day ‘cure’ genetic diseases.”
Additional study authors include Nicole Ali McNeer, Elias Quijano, Yanfeng Liu, Parker Sulkowski, Audrey Turchick, Yi-Chien Lu, Dinesh C. Bhunia, Arunava Manna, Christopher J. Cheng, Francesc López-Giráldez, Adele Ricciardi, Jagadish Beloor, Diane S. Krause, Priti Kumar, Patrick G. Gallagher, Demetrios T. Braddock, and W. Mark Saltzman from Yale University, and Dale L. Greiner and Michael A. Brehm from the University of Massachusetts Medical School.
The research was funded by the National Institutes of Health (R01AI112443, R24OD018259, and U54DK106857), the National Science Foundation (CHE-1609159), the DSF Charitable Foundation and the Robert E. Hunter fund at Yale University.
Originally published: https://www.cmu.edu/mcs/news-events/2016/1026-Gene-Editing-PNA.html