Shining a light on intracranial pressure
For the past several years, Jana Kainerstorfer, Assistant Professor of biomedical engineering, and Ph.D. candidate Alexander Ruesch have been developing a non-invasive method to measure intracranial pressure, the pressure in the head, which can increase to dangerous levels in the case of traumatic brain injuries. The project has recently moved to the clinic, and while it is still in the early stages, this development is a major step in the research’s overall aim to develop a novel sensor to help guide traumatic brain injury treatment.
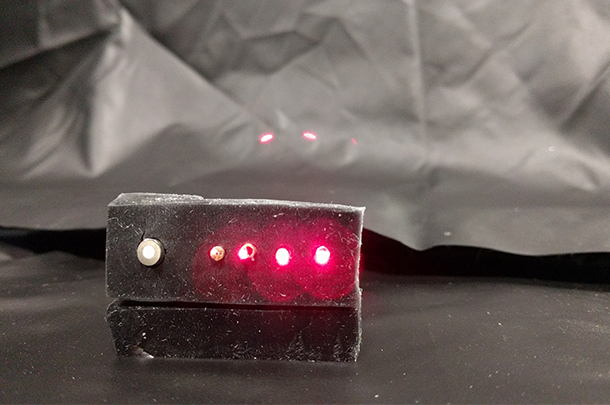
Kainerstorfer, Ruesch, are collaborating with Associate Professor Matthew Smith of biomedical engineering to develop an alternative to current practices that involve invasive surgery. Instead of drilling a hole in the skull to place a probe in the brain, they shine near infrared light into the brain, which is reflected back to the surface, and calculate cerebral blood flow. This method is called diffuse correlation spectroscopy, which the researchers have optimized to increase the speed of sampling.
“We shine light onto the head, and in this case, we’ve optimized how fast we can sample,” said Kainerstorfer. “We measure intensity fluctuations, which translate to blood flow changes within the brain. And so, every time the heart is beating, we get the cardiac pulsation.”
To analyze the intracranial pressure data, they have developed a machine learning algorithm that takes the waveform of blood flow measured with diffuse correlation spectroscopy, and translates the data into absolute numbers of intracranial pressure. Depending on the unique waveform shape, the algorithm can infer if the pressure is healthy. The methods have worked well in a pre-clinical setting, and the researchers are now translating it into the clinical environment.
They place optical fibers on the head of brain trauma patients in the pediatric ICU. As patients suffering from traumatic brain injuries or hydrocephalus, the buildup of fluid in brain cavities, they have clinical symptoms that justify standard invasive surgical measurement. By having both methods work concurrently, they hope to compare the two methods and analyze the results. Clinical translation into the pediatric ICU at the Children’s Hospital has been possible due to dedicated clinical collaborators, including Dr. Elizabeth Tyler-Kabara, Dr. Robert Clark, Dr. Jaskaran Rakkar, and Dr. Michael McDowell.
“What I’m hoping for is taking the methods that we develop to determine who has elevated pressure, such that it is a more quantifiable way that goes beyond clinical symptoms of justifying who needs a pressure probe,” said Kainerstorfer.
The pre-clinical results have been published recently and Kainerstorfer has received funding to continue their research from the Pennsylvania Infrastructure Technology Alliance (PITA) and the Center for Machine Learning and Health (CMLH), a joint partnership between Carnegie Mellon, the University of Pittsburgh, and UPMC.