Search:
Browse directory
Filter
- All
- advanced manufacturing
- bioengineering
- computational engineering
- energy
- environmental engineering
- machine learning
- micro/nanoengineering
- product design
- robotics
Faculty
-
-
-
Sarah Bergbreiter
Professor, Associate Head for Strategic Initiatives
-
-
-

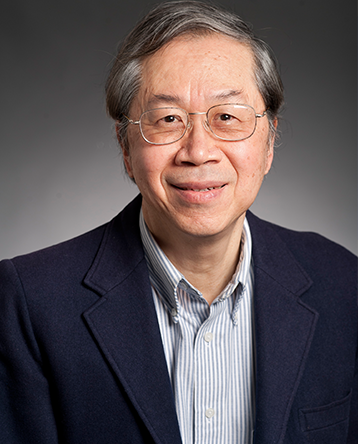
Jonathan Cagan
David and Susan Coulter Head of Mechanical Engineering
George Tallman and Florence Barrett Ladd Professor
Associate Director, Human+AI Design Initiative -
-
-

Diana Haidar
Faculty Director, Tech Spark
Associate Professor of the Practice -
-
-
-
-
-

Levent Burak Kara
George Tallman and Florence Barrett Ladd Professor
Associate Head for Academic Planning -

Philip LeDuc
William J. Brown Professor
Director, Center for the Mechanics and Engineering of Cellular Systems
-
-
-
-

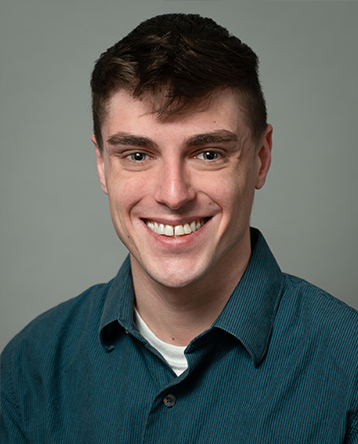
Christopher McComb
Gerard G. Elia Associate Professor
Director, Human+AI Design Initiative -
-
-

Burak Ozdoganlar
Ver Planck Professor
Associate Director, Engineering Research Accelerator
Co-director, Pennsylvania Infrastructure Technology Alliance (PITA)
-

Rahul Panat
Professor
Associate Director of Research, Manufacturing Futures Institute
-
-
-
-
-
-
-
-
-
-
-
-
Associated faculty
Courtesy faculty
-
-

Peter Boatwright
Allan D. Shocker Professor of Marketing and New Product Development
Co-Founder & Co-Director, Integrated Innovation Institute
-
-
-

Gary Fedder
Howard M. Wilkoff Professor
Faculty Director, Manufacturing Future Institute
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-

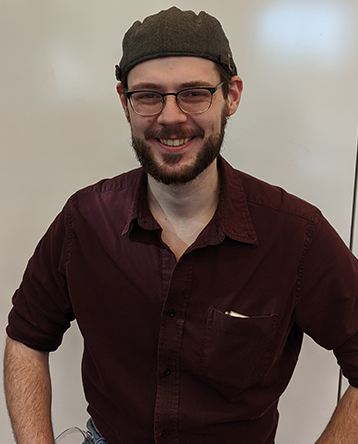
David Wettergreen
Research Professor
Associate Director for Education and Director of the Ph.D. Program
-
-